Knowing my blood sugar (glucose) levels is key to maintaining a healthy lifestyle with type 2 diabetes, as well as preventing long-term health complications. My health care provider recommended checking my blood sugar two times a day. I check my blood sugar levels each morning, before breakfast, known as a fasting blood sugar, and again at night 2 hours after dinner. Each diabetic’s journey is different, work with your health care provider to identify when to check your blood sugar each day. I also check my blood sugar when I feel my level could be too low or too high, or when introducing new foods that may affect my levels.
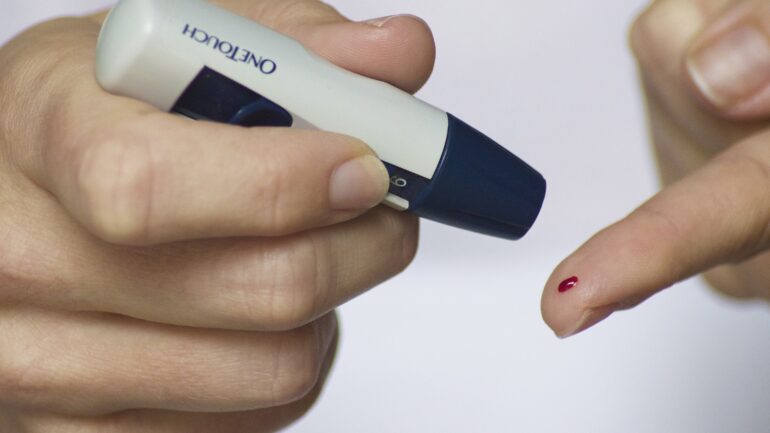
My health care provider prescribed a blood glucose monitor for my home blood sugar checks. The monitor my provider prescribed is known as a traditional (or invasive) glucose meter. These monitors are considered the most commonly used device for home blood glucose monitoring, they are also considered the most accurate device. Although somewhat intimidating at first, this monitor has met my needs.
These monitors generally come as a testing kit, which includes the monitor, lancet device, lancets, test strips, and controls. You will need to purchase additional lancets, test strips, and controls, as you use the device.
How to Check Your Blood Glucose At Home (using a traditional monitor):
Take time to become familiar with your glucose monitoring kit. Read the instructions and understand how your personal glucose monitor operates. Set your monitor’s date and time to ensure the internal log is accurate.
Your blood glucose monitor should come with a picture diagram to help you accurately check your blood sugar levels. Here are general instructions on how to check your blood glucose at home:
- Wash and dry your hands completely to prepare for testing. If soap and water aren’t available, keep an alcohol pad with your monitor to clean the testing site. The foods and oils on our hands can cause an inaccurate result.
- Prepare your lancet device by placing the lancet in the device, push the lancet into place to engage the needle, and twist off the safety cover. Recap the lancet device and choose the appropriate setting for needle depth based on your skin type. A low setting is best for thinner skin and a higher setting is best for thick or calloused skin.
- Taking a test strip from your storage container, place the strip into your glucose meter. Recap the storage container. Your meter will prompt you when it is ready for a blood sample.
- To obtain the blood sample, press your lancet device to the side of your fingertip and press the button on your device to prick your fingertip with the needle (lancet). The middle and fourth fingers are typically the least sensitive, however any finger can be used. Some devices will recommend pricking an alternative location, such as the palm or forearm. Fingertips generally provide the most accurate reading.
- Rub from your palm and down your finger to the testing site on your fingertip to increase the sample of blood. Keeping your finger below your heart, take your meter at an angle and touch the end of the test strip to the drop of blood until the blood flows up to the sensor of the testing strip.
- The meter will display your blood sugar level on a screen after a few seconds. If you receive an error code, check your user manual and retest. Common errors include issues with the testing strip or inadequate blood sample.
- Remove the lancet from your lancet device. To dispose recap and dispose if possible, otherwise place the lancet in a secure container to dispose or place in a medical waste sharps container,if available. Manufacturers recommend discarding lancets after each use.
Record your blood sugar results including the date and time, as well as any other information such as before or after meals or the time you took your medication. This will help you better monitor your progress. Also, many health care providers will want to review this information with you at your next appointment.
Here are some tips for ensuring you have accurate blood sugar readings:
- Store your blood glucose monitor and supplies based on manufacturer’s guidelines.
- Use the appropriate testing supplies, ensure your supplies are not expired.
- Run quality checks as directed, most kits will come with quality control liquid. Follow the instructions for running the quality control, the appropriate range for results will be on the bottle of your test strips.
Alternative Blood Glucose Monitors
Traditional monitors continue to be the most popular device for testing blood sugar levels, however new technologies have entered the market in recent years. Although not as accurate, these new technologies provide less discomfort and more convenience for patients.
Non-invasive Glucose Monitors
Technology has advanced replacing the need for daily finger pricks. Non-invasive glucose monitors use physico-chemical sensors on the skin to analyze molecules from the skin using an electric current. Although being used in some countries, this relatively new technology is still in development and at this time not as accurate.
Continuous Glucose Monitors (CGM)
A continuous glucose monitor or CGM is a monitor that is inserted under the skin’s surface. The monitor is worn at all times and measures your blood sugar every few minutes. The blood sugar levels are sent to a receiver and/or application on your smartphone or smartwatch. Depending on the CGM system, sensors are typically worn for a few weeks or few months before they need to be changed. Many CGM systems have an alarm that will alert you if your blood sugar is going up or down too quickly, others require you to check your blood sugar levels in on the receiver or application periodically.
Work with your health care provider to identify the best monitor for you. Carefully weigh your personal needs and preferences including ease of testing, frequency of testing, and financial considerations.
Whether you are using traditional blood glucose monitoring or new advanced technologies, it is important for blood sugar monitoring to become part of your daily routine. Maintaining a log of your daily blood sugar readings helps you better understand your blood sugar levels and control your diabetes. Access my easy to follow Blood Glucose Chart here.
If you have questions about monitoring your blood glucose, I encourage you to reach out to your health care provider. Many insurance companies cover portions of the cost of blood glucose monitors. Contact your health care professional or pharmacy to inquire if there are additional financial resources.
How have you made monitoring your blood sugar levels part of your daily routine?